By Dr. Derek Ochiai
“A field hockey player is on a breakaway, with only one defender to beat before a clear shot to the goal. She makes a cut, and suddenly feels a pop in her knee, and she falls to the ground. The knee swells up, and the sports medicine doctor notes looseness in her knee. She gets an MRI, which shows an ACL tear, and the news is understandably devastating.”
In the above scenario, typically the recommendation in 2017 would be rehabilitation to regain range of motion and strength in the knee. If the athlete wants to continue sports that involve change in direction and twisting, usually surgery is then recommended. Most of the time, ACL reconstruction (using a tendon graft) is the recommended surgical treatment. However, there are some ACL tears that can be repaired, strengthening and reinforcing the patient’s own ACL, with potentially a faster healing process.
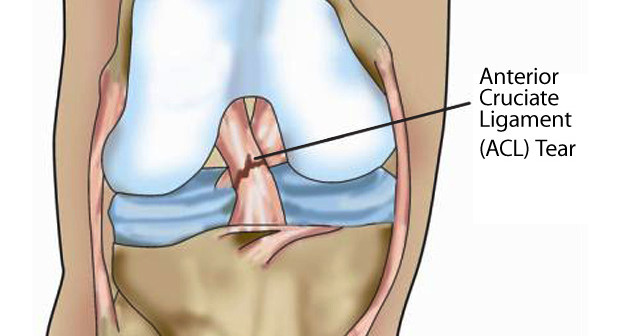
What is the ACL?
The ACL (anterior cruciate ligament) is one of the major stabilizing ligaments of the knee. It sits in the middle of the knee, and helps to control rotation.
How does an ACL tear?
Many times, ACL tears are non-impact, meaning that the athlete’s knee or body was not hit by another player or object. With quick change in direction, the stress on the ACL is overloaded, and a tear occurs. Other times, the athlete’s knee may be clipped by another, forcibly hyperextending the knee.
What are the symptoms of an ACL tear?
Initially, the athlete will usually fall or collapse because of the tear. Many times, they can leave the field under their own power (it is wrong to assume that an athlete who walks off under their own power does not have a significant knee injury). The knee may feel wobbly or unstable, or just “feel wrong”.
How is it diagnosed?
The athletic trainer or sports medicine physician will do specialized tests to see if the ACL is not working properly. The most common is a Lachman Test, which tests knee stability when the patient is relaxed and the knee is slightly flexed. The most specific test for ACL tear is the Pivot Shift Test, which tests the rotational stability of the knee (which is compromised by an ACL tear). Typically, X-rays are obtained to make sure there is no bony fracture of the knee. An MRI is usually obtained, which shows the torn ACL (Figure 1).
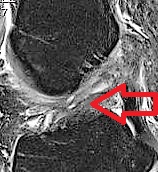
Figure 1: MRI showing an irreparable mid-substance ACL tear. Notice how wavy the ACL is throughout the entire ligament.
What are the treatment options for an ACL tear?
Depending on the athlete and the mechanism of injury, some ACL tears can be treated conservatively, and the athlete feels OK. The ACL tear will not heal on its own, but the athlete can deal with the instability. For many athletes who want to go back to aggressive sports, surgery is usually recommended. ACL reconstruction is currently the gold standard for treatment of ACL tears. This involves a tendon graft used to replace the torn ACL. The graft sits in sockets in the femur and tibia, and the graft is held in place while it heals.
Recently, ACL repair has emerged as an option for ACL tears that have torn off the bone of the femur. While not attached to the femur, the ACL itself has good tissue integrity, and if it heals, the ACL can function normally. If the tear is amenable to repair and if the injury is addressed relatively quickly, then ACL repair is an option.

Figure 2. This MRI shows a repairable ACL tear. Note how the black fibers are in continuity, and just avulsed off at the top.
Why repair the ACL?
ACL repair might be preferable to reconstruction for a number of reasons. First, repairing an ACL restores normal anatomy. While an ACL reconstruction makes the knee stable, it is using a tendon to recreate a ligament, which is not “normal”. The ACL has a blood supply and nerve supply, which can aid in proprioception. An ACL reconstruction graft does not have these. Finally, ACL repair may result in a quicker return to sport than ACL reconstruction.
I thought ACL repairs didn’t work?
Back in the 1960’s and 1970’s, surgeons would try to repair the ACL. However, the techniques used to “repair” are not anything close to what arthroscopic sports medicine surgeons have at their disposal now. Back then, repair was basically using low strength suture to re-approximate the ends of the ligament. There were no such things as suture anchors to repair ligament to bone. Modern ACL repair techniques take advantage of technology that has been used to successfully repair other tendons and ligaments, such as the rotator cuff. Remember, there were reputable doctors and scientists who contended it was impossible to run a four minute mile, and now high school runners are beating that mark!
How do I know if my ACL tear is repairable?
First, if you are feeling instability in your knee, you should be assessed by a sports medicine physician, to see if you have an unstable ACL. In this particular instance, it would be preferable to get an MRI relatively quickly, since ACL repair is better done in the acute setting (chronic ACL tears will result in tissue degeneration and scarring down of the stump of the ACL, making ACL repair either more difficult or not an option anymore). The MRI should be read by a sports medicine surgeon who could possibly repair the ACL, since just reading a report that says “torn ACL” does not indicate whether or not the ACL tear is repairable.
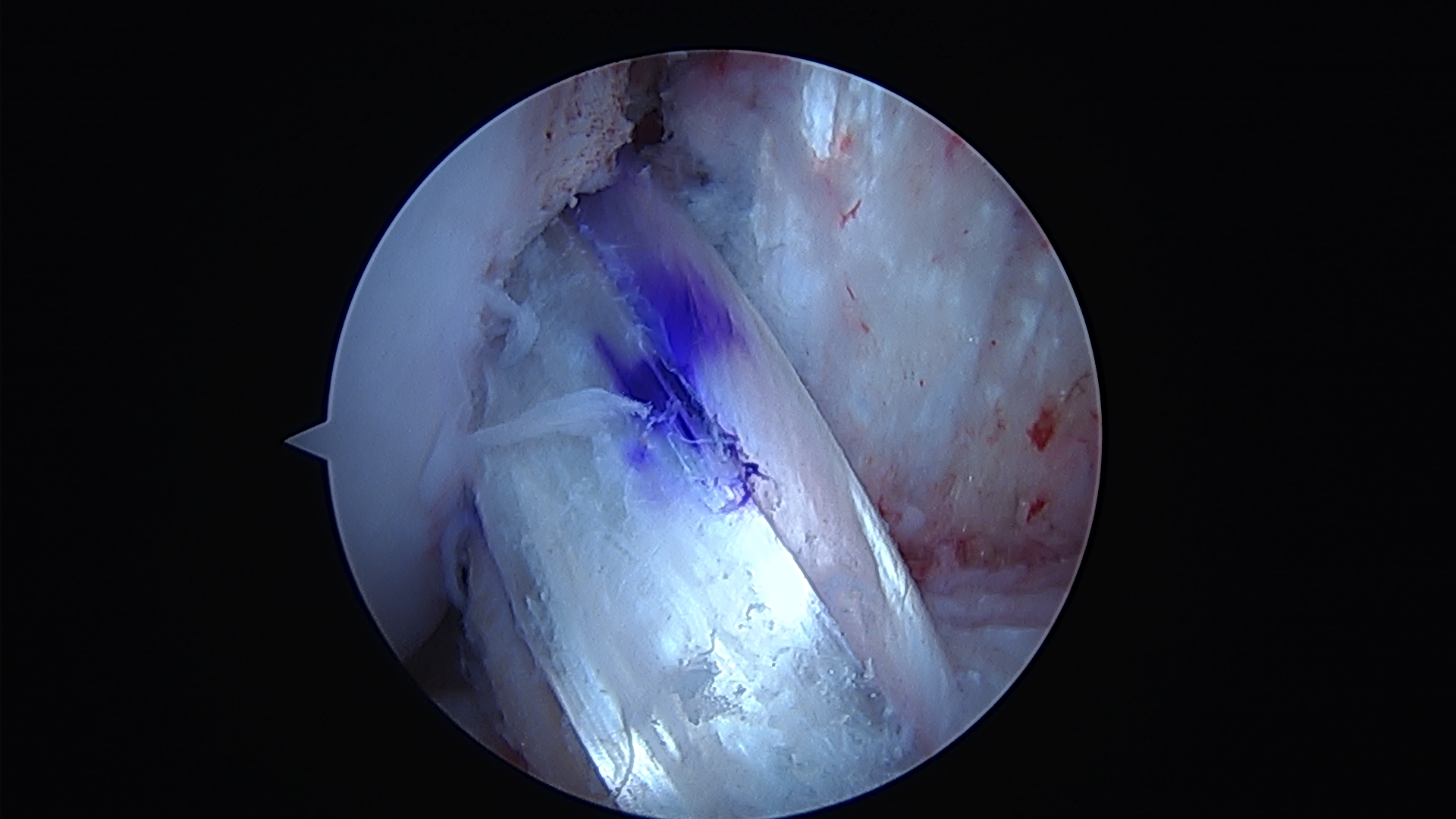
Figure 3. Arthroscopic image of an ACL reconstruction using a hamstring tendon graft.
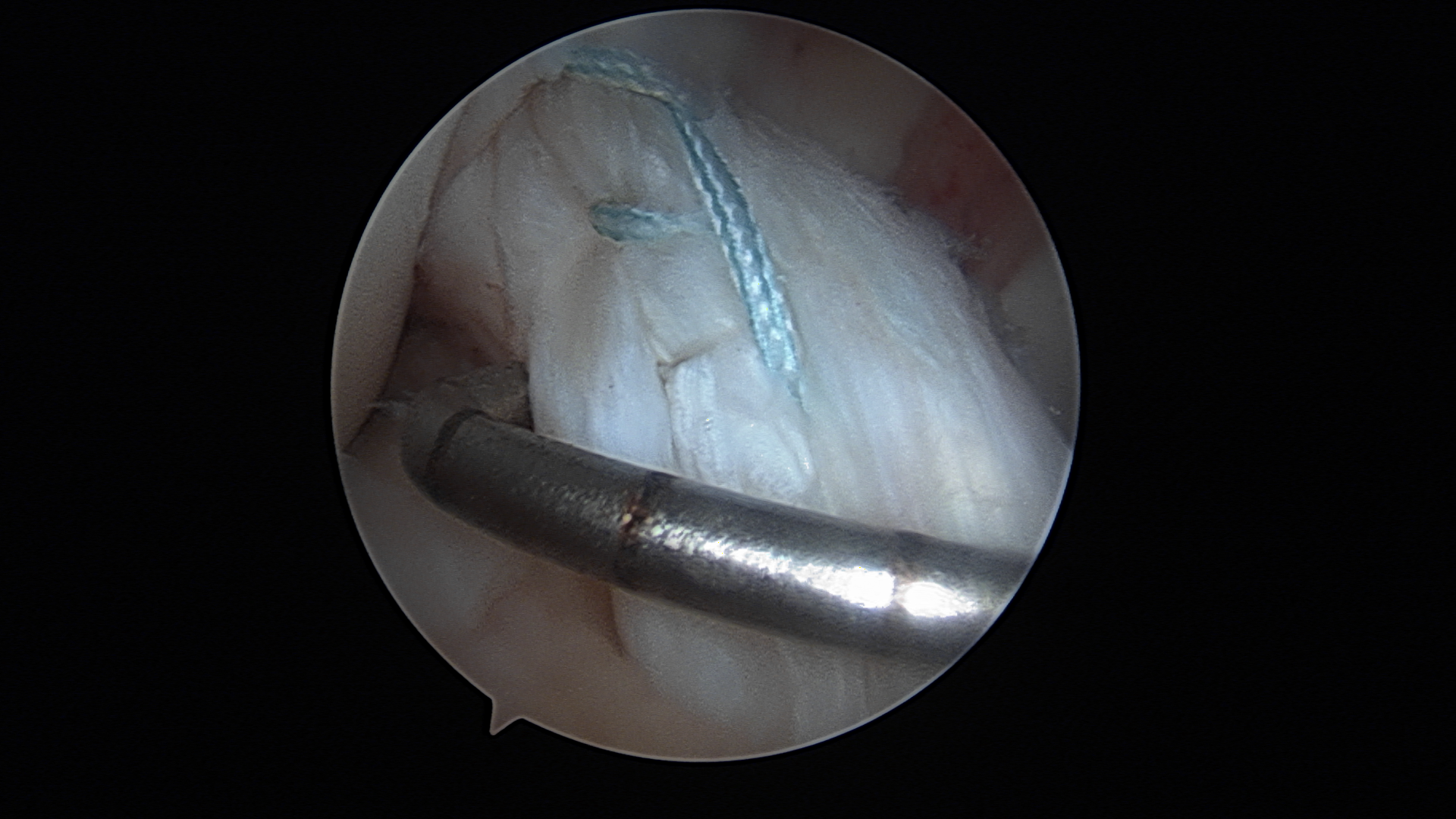
Figure 4. Arthroscopic image of an ACL repair using suture anchors.
In conclusion, many ACL tears in athletes require arthroscopic surgery. In 2017, the options for surgery could be either ACL reconstruction or ACL repair.
Dr. Derek Ochiai is a Hip Arthroscopy and Sports Medicine surgeon at the Nirschl Orthopaedic Center. Follow him on Twitter: @DrDerekOchiai